Clinical Conditions
Prolapse:
What is Pelvic Organ Prolapse?
Pelvic organ prolapse is the loss of pelvic support that occurs when the soft connective tissue that support the pelvic organs become stretched, weakened or torn. It is a very common disorder, particularly in older women.
While aging is a factor, there are many potential contributing causes. They include loss of muscle tone, menopause and estrogen loss, multiple vaginal deliveries, obesity, uterine fibroids, family history, pelvic trauma or previous surgery, repeated heavy lifting, chronic constipation and coughing and certain medical conditions such as diabetes.
Did you know…
Half of all women over age 50 experience some degree of pelvic organ prolapse. Twenty percent of women over 60 years of age will require surgical intervention.
Mr Fiadjoe and his team have specialist expertise in treating women with prolapse and see many patients each week with this problem.
Common symptoms include:
- Feeling a lump / swelling in the vagina which may be uncomfortable
- A dragging or dropping sensation
- Backache
As the bladder or bowel may prolapse into the vagina, it is quite common for women to develop other symptoms such as incontinence, difficulty emptying and urgency although not everyone is affected in this way. Some patients also find that intercourse is uncomfortable or they don't get enough sensation – the prolapse can also put them off having sex. Severity of prolapse are generally described as mild, moderate and severe.
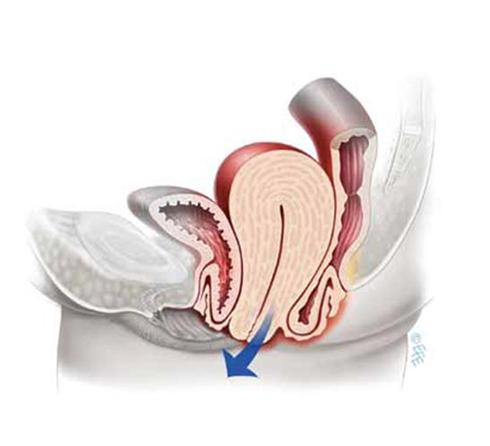
Types of Prolapse
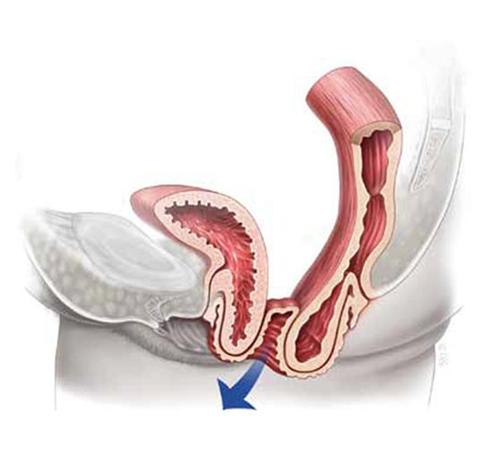
Weakness of the surrounding supports along with the muscles can lead to several different types of prolapse including;
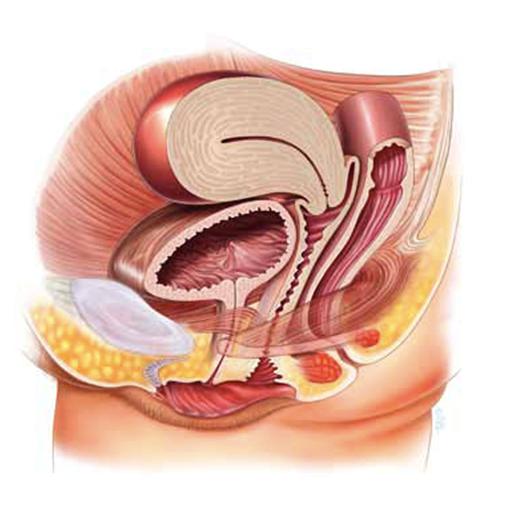
Normal Anatomy
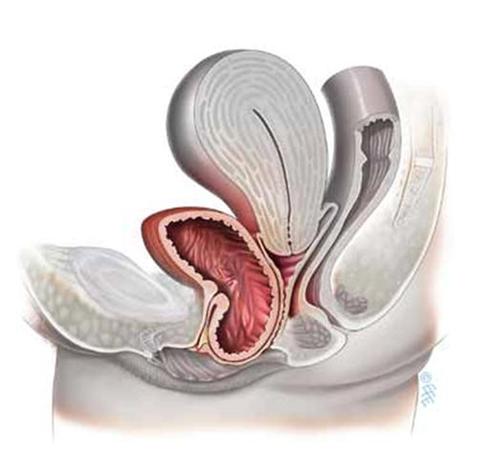
Bladder prolapse also known as cystocoele
Bowel Prolapse also known as Rectocoele
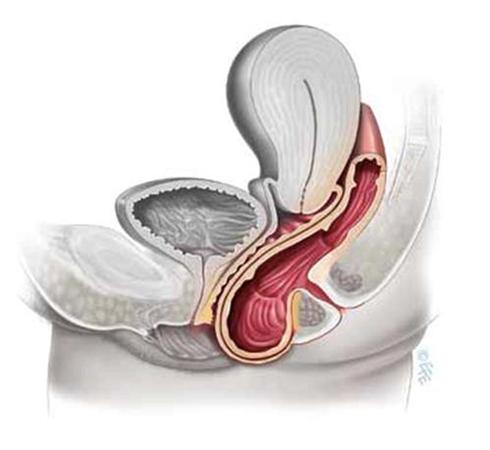
Womb Prolapse- Uterine prolapse
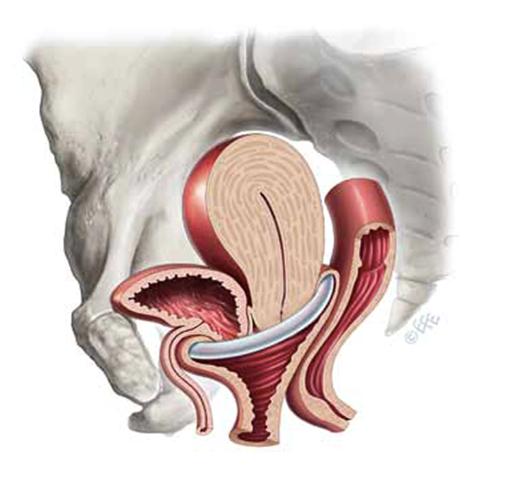
Top of the vagina: Vault Prolapse. This is a woman who has had a hysterectomy.

Normal vagina vault
Vault Prolapse
Back to Top
Treatments:
No Treatment
Not everyone with a prolapse will need treatment. Many women will be found to have a weakness of the vaginal walls or prolapse (perhaps when they have an examination or go for a smear test) and have no symptoms at all. They usually don't require any treatment but should probably try to avoid a lot of heavy lifting or straining as this can make things worse.
Physiotherapy
Pelvic floor exercises (e.g Kegel's exercise) may help and these can be taught by the physiotherapy teams at Springfield or Broomfield Hospitals.
When performing incontinence or prolapse treatments, concentrate just on the pelvic floor muscles and do the best you can. This contraction will get easier with practice. One exercise program is described below:
- Identify the correct muscles that are to be exercised.
- Attempt to contract and hold the muscle squeeze for 10 seconds
- Relax for a period of 10 seconds
- Perform 10-15 contractions and relaxation
- Perform this regimen 3-4 times a day
By faithfully doing your Kegel exercises, you should see an improvement in your symptoms starting in four to six weeks.
Vaginal cones are sometimes used to help with pelvic floor exercises. Vaginal cones are miniature weights which are placed into the vagina and help women achieve stronger pelvic floor.
Pessaries
Some women prefer to use a pessary – which is a plastic device which sits in the vagina and stops the uterus or walls of the vagina dropping down. This is usually changed every 6 months and is particularly useful for elderly patients or those keen to avoid surgery.
There are several types of pessary but rings are the most common (see picture opposite). There are several different sizes and once fitted most women feel more comfortable, although they do not suit everyone.

Ring Pessary
Vagina with Pessary in place
Back to Top
Surgery
The majority of women with a prolapse which is bothering them will choose to have an operation. The type of procedure necessary will obviously depend on the type of prolapse – this will usually be determined by a vaginal examination. Mr Fiadjoe is happy to provide a detailed assessment and performs all surgeries himself.
The following information provides a general outline for women who require vaginal surgery for their prolapse. Click here for information sheet.
We are also able to offer advanced techniques for women with recurrent problems or those with a prolapse of the top of the vagina (vaginal vault prolapse) using synthetic mesh.
For further information about recovery following surgery, please visit www.rcog.org.uk/recovering-well, and click on pelvic floor repair.
Back to Top
Urinary incontinence
Urinary incontinence (leakage) refers to the involuntary loss of urine from the bladder, which constitutes a social or hygienic problem for the individual. Bladder control problems affect about 17 million people in the United States. It can be a cause of anxiety, social embarrassment and may limit ones social and daily activities. Fortunately, most of these conditions can be treated. However the first step to curing this condition is acknowledging the problem and then deciding to see a physician who has been properly trained in treating the condition of incontinence.
There are many causes of urinary incontinence. Some of the causes of incontinence are related to temporary conditions. Once they are treated, the incontinence usually goes away. Temporary causes include:
- Urinary Tract Infection
- Constipation
- Certain medications
- Increased dietary intake of caffeine, alcohol, artificial sweeteners and carbonated beverages
- Some other causes of incontinence are not temporary. There is, however, treatment available for many of these conditions. Other causes of incontinence include:
- Weakness of the muscles that hold the bladder in place
- Weakness of the bladder sphincter muscles
- Overactive or under active bladder muscles
- Neurological disorders (ex: Multiple Sclerosis, Parkinson's Disease, Stroke)
Mr Fiadjoe and his team see at least 15 women each week who are having regular urinary leakage. Our sympathetic and understanding approach aims to put women with this often embarrassing condition at their ease.
A full range of treatment options are available including pelvic floor physiotherapy, medication and surgery – which is most often performed as a day case with a short recovery time.
Many women with incontinence will also have other problems such as prolapse or heavy periods. As Mr Fiadjoe is a Urogynaecologist he can treat both bladder problems and gynaecological problems at the same time.
Back to Top
Type of Urinary Incontinence:
Stress Urinary Incontinence
Stress incontinence is the loss of urine during coughing, sneezing, laughing or lifting something heavy. These activities cause an increase in "belly pressure", which forces the urine out of the bladder. Some patients suffering from stress incontinence will leak only a few drops while others may leak more than a cup. Stress incontinence occurs almost exclusively in women and is thought to be due to "pelvic (vaginal) relaxation" from childbirth or aging. Excessive weight can be a contributing factor. Patients suffering from stress incontinence may experience:
- Leakage of urine when coughing, sneezing, or laughing
- Frequent trips to the bathroom in order to avoid accidents
- Reluctance to exercise to avoid accidents
- Sleeping through the night but leaking when getting out of bed in the morning
- Leakage upon rising from a chair
Urge Urinary Incontinence
Urge incontinence occurs when someone cannot delay the bladder's message to empty. When this type of incontinence occurs, the person often experiences "the urge" and often the individual cannot make it to the restroom on time. Urge Incontinence is the most common type of incontinence and is usually readily treated with medication. Patients suffering from urge incontinence may experience:
- Difficulty maintaining their urine on the way to the bathroom
- Getting up frequently during the night to urinate
- The need to go to the bathroom at least every two hours
- Feeling of a weak bladder or a small bladder
Mixed Incontinence
Many patients have a combination of incontinence types. Especially prevalent are patients with both stress incontinence and urge incontinence. These patients experience symptoms of:
- Leakage with cough, sneeze and rise of abdomen pressure
- Leakage which is sudden and with little warning
- Frequent daytime urination
- Urgency
Back to Top
Investigations
Sometimes it is possible to determine why someone is leaking based on their symptoms and an examination. However, it may be necessary to perform some tests to gain more information which will show which treatments will be required. These include:
- A urine sample – to exclude infection, diabetes and blood in the urine
- A bladder diary – information regarding how many times a patient passes urine and the amount they drink can be really useful. If possible it helps to complete a bladder diary for a couple of days and then bring this to you first appointment. Click here for Bladder Diary information sheet.
- Urodynamics – It is not necessary to perform this test in all patients but urodynamic studies do provide lots of information about why someone is leaking, and may detect the cause of other symptoms such as urgency or difficulty emptying. Click here for Urodynamic Studies information sheet.
Back to Top
Treatment of Urinary Incontinence:
Stress Urinary Incontinence
- Pelvic Muscle Training
- Surgery
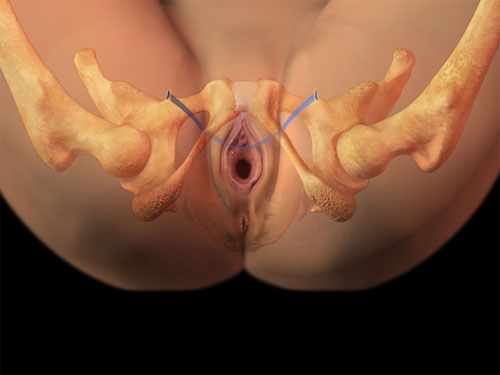
Transobturator Sling (TOT) (image above)
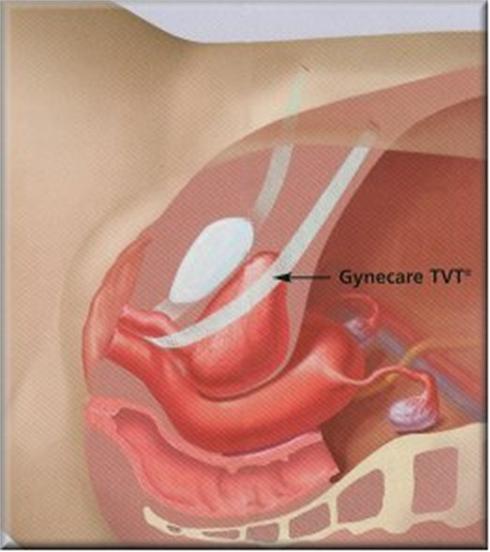
Tension Free Vaginal Sling (TVT) (image above)
- Urethral Bulking Agent
- Burch Colposuspension
- Pubo-vaginal sling
Back to Top
Overactive Bladder (Urgency Urinary Incontinence)
- Fluid and Caffeine management
- Bladder retraining
- Anti-muscarinics drugs
- Intravesical Botox injection (patient’s who have failed other forms of treatment)
Back to Top
Other Bladder problems
Women of all ages have can have problems with their bladder. Common symptoms include:
- Frequency – going to the toilet more often than you would like to
- Nocturia – having to get up to pass urine during the night
- Urgency – having to rush to the toilet
- Incontinence – leaking urine (Click here for information on incontinence)
Mr Fiadjoe has expertise in treating all these conditions and would be happy to help if you are having one of the above problems or other concerns. To make an appointment please click here or feel free to contact us.
Urinary Urgency
Urgency is when a patient develops a sudden, compelling feeling that they want to pass urine. Sometimes the urgency can be so powerful that urine starts to leak before reaching the toilet – a condition called urge incontinence. Many women notice that these problems occur when they listen to running water, wash their hands or put their key in the door.
Common causes of Urgency
Often urgency occurs because the bladder is irritable or overactive – a condition known as detrusor overactivity. However, there are a number of other common causes of frequency and urgency:
- Drinking too much (or too little) fluid
- Caffeinated drinks (e.g.) coffee and tea
- On overactive bladder(Click here for information on urge incontinence)
- Urine infection
- Prolapse
- Lack of oestrogen after the menopause
- Medication (e.g.) diuretics / water tablets;
What Treatments are available
- There are ranges of treatments available depending upon the underlying cause. Mr Fiadjoe is happy to discuss these in detail.
Back to Top
Cystitis/ Recurrent Urinary tract Infection
Women are much more likely to develop cystitis compared to men - mainly because their water pipe (urethra) is shorter and it is easier for bacteria to reach the bladder to cause an infection.
Common symptoms of Cystitis
- Cystitis can cause a number of symptoms including:
- Frequency
- Discomfort on passing urine
- Offensive smelling urine
- Pain in the bladder - particularly when trying to hold on.
What treatments are available?
- A number of simple treatments can sometimes help:
- Drinking a reasonable amount of fluid each day
- Cranberry juice - a couple of glasses each day can help prevent bacteria from growing in the urine
- Good hygiene - although excessive washing does not help
- Passing urine after sexual intercourse
- Acid free diet
Often a urine sample will confirm an infection and a course of antibiotics will clear the problem. However, many women will go through a phase where they have frequent infections and require several courses of antibiotics. Investigations to look for an underlying cause may be needed - these include ultrasound, X-ray and flow tests to make sure the bladder is emptying properly. Sometimes it is also necessary to perform a Cystoscopy to look inside the bladder.
Is cystitis always caused by infection?
Cystitis can occur even when there has been no definite infection - or when infection has been suspected but repeated urine samples are clear. This is often due to inflammation or soreness of the skin inside the bladder. Mr Fiadjoe is happy to help in these circumstances and can offer a variety of different treatments.
Back to Top
Heavy Menstrual Periods (Menorrhagia)
Almost one third of women are affected by heavy menstruation at one stage in their lives. This can affect women of all reproductive ages, from teenagers to the age of the peri-menopause (the time period around the menopause). Some women also suffer from pain with their periods, and both can have a significant impact on quality of life. Women with heavy periods can also suffer from generalized weakness and anaemia, with significant impact on work and family life.
I advise women initially to keep a menstrual diary to see if the pattern of bleeding is regular or irregular. For women above the age of 45years, I take a small sample from the lining of the womb called endometrial biopsy (sample). This can normally be done in the outpatient clinic. In addition, I will organize for an ultrasound scan of the pelvis to assess the size of the uterus and the presence of fibroids or polyps, as fibroids can be an important cause of heavy bleeding.
For heavy regular periods, I advise women to try tablet treatment first that can reduce the heaviness of the bleeding with the period. If the bleeding pattern is irregular, it is important to try to regulate the periods with other tablets containing Progesterone (Norethisterone or Provera). These tablets can be taken from day 5 to day 21 of the period to stop the bleeding between periods.
If the above treatment fails, a medicated uterine contraceptive device called the Mirena IUD can be inserted (see picture). This contains Progesterone and releases it slowly in the womb to thin the lining of the womb and reduce the heavy menses. It normally takes up to 6 months to reach maximum benefit, during which women might experience irregular vaginal bleeding.
If the above conservative treatments failed, then I discuss surgical options for treatment of women with heavy periods, which include endometrial ablation and hysterectomy. For more details see under patient information leaflets.
Back to Top
Pelvic Pain
Mr Fiadjoe treats women with painful periods and pelvic pain. He has expertise in the laparoscopic (keyhole) treatment of endometriosis and treats many women each year using Laser surgery in addition to a range of other medical therapies.
There are a number of causes of pelvic pain and often investigations, such as ultrasound, are necessary to make an accurate diagnosis. Common problems include:
- Endometriosis
- Ovarian cysts
- Infection
- Adhesions (scarring) from previous surgery
- Bowel problems (e.g.) constipation
- Bladder problems (e.g.) cystitis or urinary tract infection
Many women have a combination of symptoms such as painful periods, discomfort on sexual intercourse and some problems with their bladder. As Mr Fiadjoe is a Urogynaecologist he can treat both gynaecological and many urological symptoms at the same time.
Endometriosis is a common cause of pelvic pain particularly in women who are having periods. This a condition in which the inner lining of the womb (the endometrium) can start to grow on the outside of the womb, walls of the pelvis or ovaries. Although it may cause no problems in some women, many patients can have quite severe discomfort and find it affects their sex life and ability to conceive. More information about endometriosis can be found at http://www.endometriosis-uk.org/information.html

Childbirth Trauma
Perineal trauma is any damage to the genitalia during childbirth that occurs spontaneously or intentionally by surgical incision (episiotomy). This can result in an injury to the labia, anterior vagina wall, urethra, clitoris, posterior vaginal wall, perineal muscles, or anal sphincter.
More than 85% of women having a vaginal birth sustain some form of perineal trauma and 60-70% will receive stitches.
Perineal trauma affects women's physical, psychological, and social wellbeing in the immediate postnatal period as well as in the long term. It can also disrupt breastfeeding, family life, and sexual relations.
7-10% of women continue to have long-term pain, 23% of women experience painful intercourse at 3 months, up to 24% have urinary problems and 3-10% report faecal incontinence.
Mr Fiadjoe is a specialist in perineal trauma and runs a special clinic to help women with ongoing problem.
Please do not suffer in silence!
Back to Top





